Genetics 101! Happy New Year, HHT Community!

I thought I would use this time and space to update you on the newest Friday family addition, our son, Theo! Theodore was born last month and came out a healthy, hefty bundle of snuggles and cuteness. Our life has been a giant blur of moving to a new duty station, having a baby, chasing a toddler, and changing a lot of diapers! In between all this, of course, have been the appointments to address the not-so-fun part of our lives… HHT.
Eleanor was diagnosed with HHT January 2017 and her little brother Theo was just diagnosed this month. They are wearing their happy organ shirts given to them by their Aunt Abby and Uncle Joe! We hope for happy organs for them both as they go through their journey with HHT.
I recently joined the HHT community groups on Facebook and I have seen a lot of questions about genetic testing. Since we are going through this process with Theo, I thought I would write a bit about it. We have been working with Matthew Thomas, a genetic counselor from the University of Virginia Health System. He was able to set up a blood draw for Theo, get the blood sent to Ambry (a genetic testing laboratory), and also consult us about his results. Unfortunately, Theodore also has HHT.
The genetics can be pretty confusing, especially if this is your first go-around with testing or getting a diagnosis. Let’s use a couple of imaginary families to introduce some of the basic genetics of HHT.
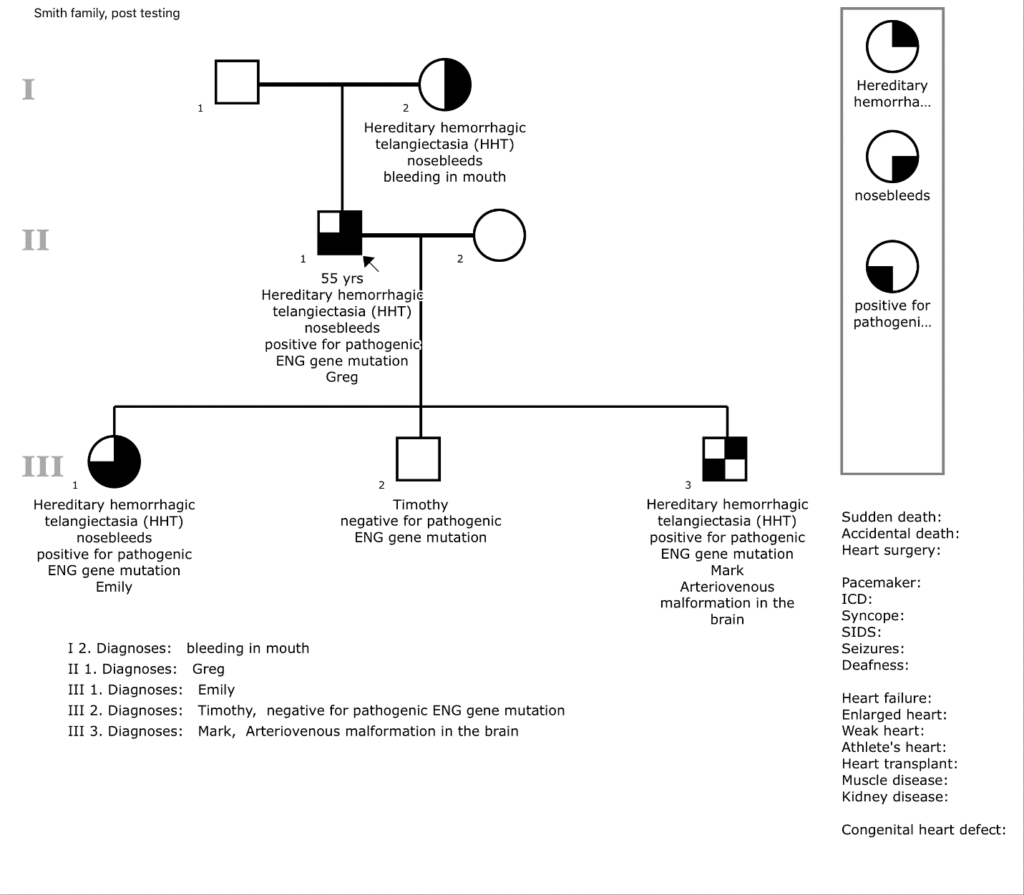
Greg Smith, a 55-year-old father of three, has had nosebleeds daily throughout his life. His mother had frequent nosebleeds and bleeding in her mouth. One of his children also has occasional nosebleeds. The Smith’s family physician diagnosed the family with HHT based on their symptoms and referred them to a genetic counselor to get genetic testing and more information.
The genetic counselor spoke with Greg about his family members and began to draw what is called a family pedigree. This is a version of a family tree that can show which members of the family may be affected by a disease. Based on symptoms, the counselor can assume Greg’s mother, Greg, and his daughter are affected by HHT – each generation of the Smith family.
The genetic counselor describes HHT as an autosomal dominant disease. Genetic material, or DNA, is located on our chromosomes. Every cell has 23 pairs of these chromosomes. 22 pairs of these chromosomes are known as autosomes. The 23rd pair are sex chromosomes (males have an X and Y chromosome, while females have two X chromosomes). The genetic information, or genes, that cause different forms of HHT are located on these autosomes. For HHT, even if one of the two autosome copies has a mutation, it dominates over the normal autosome and causes the disease. When Greg had children, one of each pair of his chromosomes was passed along to his kids. For a person with HHT, there is a 50% chance of passing on the autosome with the mutation. That is why HHT is called an autosomal dominant disease and is passed from generation to generation.
Greg is urged to get a genetic test done to see which genetic mutation his family has that causes HHT. Depending on which mutation he has, he may have an increased likelihood of certain symptoms. For example, HHT type 1, which is a mutation in the ENG gene, tends to cause more AVMs in the lungs and brain compared to HHT type 2, a mutation in ACVRL1, which tends to commonly cause AVMs in the liver.
Greg will be tested for all the genes that are known to cause HHT. Once his results come back, his children will only have to be tested for the gene that tested positive for an HHT mutation. He is a bit skeptical to go through the process, but the counselor said it is important for him and each of his three children to get tested. Greg asks why it is necessary to get a genetic test done when they obviously know they have HHT based on their symptoms already.
Other than diagnosing which type of HHT a family has, a simple answer is that not every person displays outward symptoms of HHT. Someone may seem healthy and have no HHT related issues, but they can still have the disease.
Greg went forward with genetic testing and had his blood drawn. The genetic counselor arranged for the blood sample to be sent to a laboratory that routinely does genetic testing. They tested Greg’s DNA and looked at a few different genes: ENG, ACVRL1, and SMAD4. These are the three primary genes that contain HHT causing mutations.
Greg’s results came back saying he was ‘heterozygous for the EX3_12del pathogenic mutation in the ENG gene’. The counselor explained to him that heterozygous means the two copies he has of the ENG gene are different from each other. EX3_12del is a deleted chunk of genetic material in one of the copies of this gene. The ENG gene makes a protein called endoglin that is involved in the formation of blood vessels. Once Greg’s results came back, each of his three children got their blood drawn and sent for genetic testing of only the ENG gene (because of Greg’s testing, the lab can narrow down where to look for HHT, making the test much more simple).
Based on symptoms, Greg’s daughter, Emily, should have the HHT mutation. However, when they got the test results back, his youngest son, Mark, also tested positive for HHT. This was a surprise to everyone because he never had any symptoms! Next, the genetic counselor worked with the Smith family to get screening done for Greg, Emily, and Mark to look for vessel malformations in the lungs and brain. Greg’s oldest son, Timothy, does not need to undergo screening because his genetic test result was negative for the ENG mutation.
Screening for AVMs is necessary, as genetic testing has some important limitations. It cannot give information about the severity of HHT or how each family member will show symptoms. This is called penetrance and HHT is a disease with varying penetrance. Luckily, the Smith family got genetic testing for their children. Even though Mark never showed signs of HHT through telangiectasias and nosebleeds, he had an AVM in his brain that was found during screening. He was able to get it removed and is doing fine! Additionally, genetic testing is important to do because the Smith children will want to know if it is possible for them to pass HHT along to their future children.
The genetic counselor was pleased with how the Smith family’s case had gone, but is counseling another HHT family with more complicated genetics. The Tucker family exhibits signs of HHT and has been referred for genetic testing. Mary Tucker, the mother with several HHT symptoms, had genetic testing first. However, her results came back with no identified mutations in any of the genes causing HHT! Unfortunately, we don’t know everything about HHT, and 10-15% of HHT families do not know which gene causes their disease because scientists have not yet found the mutation.
In this case, Mary and both her children will be screened for AVMs and monitored long-term for HHT, even though only one of her children has nosebleeds. As researchers learn more about HHT, perhaps more genes will be identified that cause the disease. The Tucker family is urged to consult with their genetic counselor in the future to see if they should revisit genetic testing as more HHT causing genes are discovered.
I hope these scenarios shed some light on the importance of genetic testing and follow-up care for HHT. The process of testing has been pretty easy (not without some insurance hiccups, of course). Next for us will be screening Theo for AVMs in his brain and lungs at the UVA. Matt and the rest of his colleagues at UVA have been very helpful in facilitating this testing for us. I’ll keep everyone updated on Theo’s results!
Matt Thomas, the genetic counselor with the Cardiovascular Genetics Program at the University of Virginia, drew up this example pedigree for the Smith family based on the scenario I laid out in this post. This is a typical example of what a genetic counselor will do with your family during the genetic testing process. You can see each of the three generations of Smiths and their shapes are colored in based on their diagnosis and symptoms.