Cancer, HHT and Avastin: What’s the Connection?
One of the things I love about Cure HHT is the focus on research and clinical trials for patients. I’d like to use this post to talk about the Avastin clinical trial, which I recently saw posted on Cure HHT’s media pages.
Before delving into the background on this drug and its potential benefits to HHT patients, let me put out a disclaimer. Please talk with your physician if you think you may benefit from participating in a clinical trial. I am not a physician, nor am I a practicing medical professional. I am a scientific researcher and this post serves the purpose to summarize information about Avastin and its potential uses for the HHT community.
If you search for bevacizumab, or its brand name, Avastin, you’ll see it’s an FDA approved drug given to cancer patients to help minimize tumor growth. Your first thoughts may be ‘I don’t have cancer. Why should I try to take a cancer drug to stop my nose bleeds? Cancer drugs are harsh and scary!’
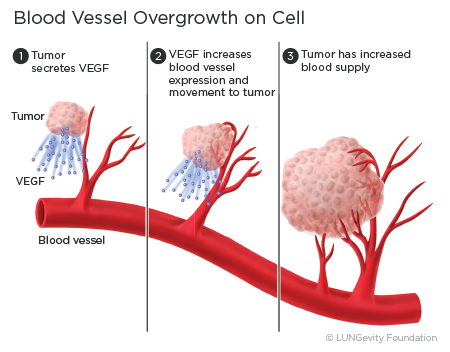 Bevacizumab is something called a monoclonal antibody, meaning it will bind to a specific target. Its target is vascular endothelial growth factor, or VEGF. In cancer, tumors secrete a lot of VEGF and it helps grow blood vessels, and therefore helps grow and spread the tumor. Bevacizumab binds to VEGF and tries to stop blood vessel formation.
Bevacizumab is something called a monoclonal antibody, meaning it will bind to a specific target. Its target is vascular endothelial growth factor, or VEGF. In cancer, tumors secrete a lot of VEGF and it helps grow blood vessels, and therefore helps grow and spread the tumor. Bevacizumab binds to VEGF and tries to stop blood vessel formation.
About 10 years ago, a couple case studies were published after HHT patients treated for cancer with bevacizumab saw dramatic improvements in the frequency and severity of nosebleeds and hepatic bleeding (Bose, Holter, & Selby, 2009; Flieger, Hainke, & Fischbach, 2006). These patients received the drug through an IV at a high dose to treat their cancer, but the unexpected benefits to HHT symptoms sparked interest in the drug as a therapy for epistaxis.
There are a lot of drugs that have had intended uses, but researchers saw positive effects on an unrelated symptom and changed the drug’s intention. Viagra, for example, was developed as a drug to treat high blood pressure and chest pain, as it dilates blood vessels. However, blood vessel dilation in other areas were a happy side effect and now the drug has a different use!
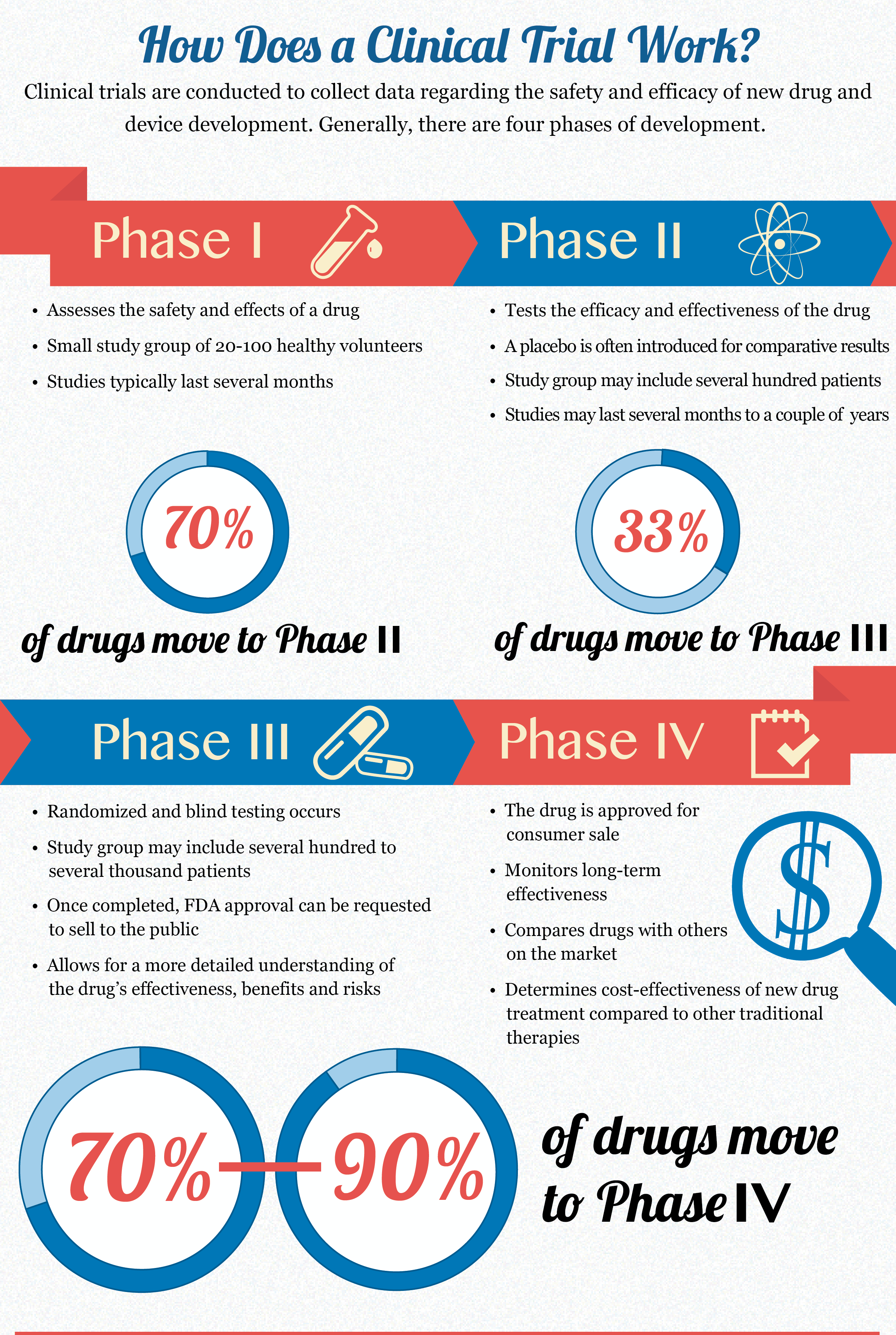
This is one of the many reasons why clinical trials are so important. Not only can a well-developed research study pinpoint good side effects, it can also pinpoint negative ones as well.
Click for enlarged image
With science, nothing is ever simple and there are always a lot of caveats. It would be great if this drug could be given in an IV and nosebleeds would get better, right? The tricky part is VEGF is something we need to be healthy, so if we try to disable it throughout our entire body, there could be other serious complications.
Researchers have tried administering the drug in a lower dose IV as well as with nasal spray, topical ointment and a submucosal injection. All have been shown to improve nosebleeds in patients with HHT, and since the dose of Avastin is so low there were no negative side effects.
Case closed, right? Well, these research studies did not directly compare its effects to a control, they did not have very many patients and some were merely case studies of a single patient (Simonds, Miller, Mandel, & Davidson, 2009; Suppressa, Liso, & Sabba, 2011; Thompson et al., 2014).
This does not mean these research studies should be discredited. They are all important pieces of information along the journey to see bevacizumab used as a treatment for HHT.
These studies and their findings led to the initiation of a clinical trial across six HHT centers of excellence comparing bevacizumab with a placebo and two other drugs in the North American Study on Epistaxis (NOSE) (Whitehead et al., 2016). In this study, patients either received a saline spray (the control for the study) or one of three drugs to spray in their nose twice a day.
 The study concluded and found there were no differences between the four groups of patients receiving the different medicines or placebo. The study lists a couple of important limitations: 1) they did not have patients keep a diary of nosebleeds before the study started, so there was no way to quantitatively compare patients before and after treatment and 2) they were not sure how effective the drug delivery was because the nose can be pretty crusty in HHT patients due to dried blood that may block the medicine’s entry.
The study concluded and found there were no differences between the four groups of patients receiving the different medicines or placebo. The study lists a couple of important limitations: 1) they did not have patients keep a diary of nosebleeds before the study started, so there was no way to quantitatively compare patients before and after treatment and 2) they were not sure how effective the drug delivery was because the nose can be pretty crusty in HHT patients due to dried blood that may block the medicine’s entry.
After all this (and much more past research), a phase IV clinical trial is now ongoing to study bevacizumab injection in the nose right after electrocautery treatment. All patients will receive electrocautery treatment, half will get an injection of bevacizumab and the other half will receive a placebo. This should ideally enhance the drug’s effects, as the nose will be cleaned of debris, cauterized and injected with the medicine.
Researchers at Stanford need several more volunteers in order to help complete this clinical trial. If you have talked with your physician, met the eligibility criteria for the study found here and are interested in helping advance the science behind this drug, I encourage you to contact the study team! If you were on the fence about participating in this trial, I hope the interesting background of Avastin has helped you make a decision!
Sources:
Bose, P., Holter, J. L., & Selby, G. B. (2009). Bevacizumab in hereditary hemorrhagic telangiectasia. N Engl J Med, 360(20), 2143-2144. doi: 10.1056/NEJMc0901421
Flieger, D., Hainke, S., & Fischbach, W. (2006). Dramatic improvement in hereditary hemorrhagic telangiectasia after treatment with the vascular endothelial growth factor (VEGF) antagonist bevacizumab. Ann Hematol, 85(9), 631-632. doi: 10.1007/s00277-006-0147-8
Simonds, J., Miller, F., Mandel, J., & Davidson, T. M. (2009). The effect of bevacizumab (Avastin) treatment on epistaxis in hereditary hemorrhagic telangiectasia. Laryngoscope, 119(5), 988-992. doi: 10.1002/lary.20159
Suppressa, P., Liso, A., & Sabba, C. (2011). Low dose intravenous bevacizumab for the treatment of anaemia in hereditary haemorrhagic telangiectasia. Br J Haematol, 152(4), 365. doi: 10.1111/j.1365-2141.2010.08481.x
Thompson, A. B., Ross, D. A., Berard, P., Figueroa-Bodine, J., Livada, N., & Richer, S. L. (2014). Very low dose bevacizumab for the treatment of epistaxis in patients with hereditary hemorrhagic telangiectasia. Allergy Rhinol (Providence), 5(2), 91-95. doi: 10.2500/ar.2014.5.0091
Whitehead, K. J., Sautter, N. B., McWilliams, J. P., Chakinala, M. M., Merlo, C. A., Johnson, M. H., . . . Gossage, J. R. (2016). Effect of Topical Intranasal Therapy on Epistaxis Frequency in Patients
With Hereditary Hemorrhagic Telangiectasia: A Randomized Clinical Trial. JAMA, 316(9), 943-951. doi: 10.1001/jama.2016.11724

Thanks Cassi
c
Could it help people with HHT in the stomach?
Hi Raymond – The clinical trial is injecting Avastin in the nose, so it is only designed to help with nosebleeds. If a person receives this antibody (bevacizumab) to their entire body in a higher dose through an IV, it may improve gastrointestinal bleeding.
https://link.springer.com/article/10.1007%2Fs00277-006-0147-8
Here is a link to a study done on a man who had HHT and also cancer that was getting worse. As part of his cancer treatment, they gave him bevacizumab and watched his HHT symptoms. As a result of the therapy, he did not require as many transfusions and his hemoglobin levels went up drastically.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5183923/pdf/WJGS-8-792.pdf
Here is another study of a woman with HHT who did not have cancer. They treated her with bevacizumab every two weeks and noticed a great improvement in her gastrointestinal bleeding and need for transfusions.
Hope this helps. I would talk to the physician who treats you for HHT and discuss the best options for you. At the low doses used in the clinical trial for nose bleeding, this drug does not have side effects. However, at high doses throughout the whole body, the drug can have some serious side effects.
I have HHT and come from a large family of HHT relatives who were never properly diagnosed. I have two offspring and one has a severe case of intestinal bleeding which began very young. We both take IV iron infusions, but they only help some. Couldn’t this drug be added to the iron infusion? I have seen more suffering from this disorder and it’s very personal, obviously, when it is family.
We both are very discouraged by the total lack of awareness among medical personnel and always must explain the disorder in detail. There are many rare disorders, but medical schools need to become better at making students aware. With anemia, we are exhausted explaining this over and over.. I have been many times to Yale, the original HHT Center of Excellence for .treatment via interventional radiology for pulmonary AVM’s.
We are grateful to Dr. Robert White for his keen interest and his interventional techniques because I had two lungs surgeries prior to being accurately diagnosed. He was wrong in thinking intestinal bleeding came later in life. My daughter started in her thirties and even had a hysterectomy to cut down on blood loss. It did not help.
I gave up iron infusions for two years because I simply gave up and became a hospice patient. My husband’s diagnosis of dementia sent me back for iron infusion so I could help him for a period of time.
It has been my objective to educate everyone in our family about this disorder and its transmission. Educating docs and dentists, some receptive some disinterested, has also been a life long task. If one celebrity had this disorder, heaven forbid, we’d have great news coverage.
We must educate physicians so HHT is instantly recognized as a serious disorder. I do not wish anyone on earth to go thru what my daughter and me have been through on this exasperating journey. There needs to be more talking between patients via the web, and I just have not found them, but am old and not that web savvy..
Some researchers are doing fabulous work. We salute them! We are going to have to fight for our moment in the spotlight. We need medical professionals and the general population educated. Let’s get to it! J. Nielsen
Very well voiced certainly! .
After many petitions to my health insurance company, the medical director has approved for me to receive IV Avastin. My doctor has chosen a low dose of 5mg/kg of body weight. I am hopeful this will not only significantly reduce the nose bleeds, but also prohibit AVM growth. Also, since I am currently anemic I will receive IV at the same time. There is no conflict between the two.
I can sympathize with all those HHT patients (because I’m right there with you) who live their life chronically anemic and requiring monthly iron or whole blood infusions. I’ll keep you posted on the results.
I’m so glad you are able to receive this treatment and I pray it makes you healthier and stronger! Definitely keep us updated.
I’m going in in December to have my nose Lasered and then several PAVM closed. 2nd time for these procedures . I then will start the Avastin infusions . I have had 20 units of blood this year so far and six iron infusions. Im hoping that the Avastin works and slows everything down. At 61 I can’t continue to get 20 units of blood.
My husband is scheduled tomorrow for IV Avastin, and iron infusion, did you have any of the side effects? I know that he’s suffered with these nosebleeds, but this drug makes me nervous for him. I hope all turned out well with you.
My husband who was diagnosed with HHT for over 40 years also had iron and blood transfusions. The nosebleeds never allowed us to have nice bed linens, shirts and all dark colors clothes were necessary. After several attempts to stop nosebleeds by a ENT physician within the HHT center under Dr. James Gossage, Augusta GA foundation, it was recommended his nose be surgically closed. This was before discovery of Avastin for HHT patients. He has completed his 4 units of avastin along with his regular iron treatments. We are excited to say his hemoglobin and his ferritin levels are within normal range for the first time since his diagnoses. Right now we live in Maine and between our wonderful team at Maine General Alfond Center Augusta and Massachusetts General HHT foundation specifically part of anemia study agreed to my husbands treatment for HHT. Now with marvelous results with all the numbers up we are concerned with now the energy levels increasing? We stay in prayer seeking the Lords work in all of this wisdom, to help improve better health for all. Glory to God
I am looking for information on nasal Avastin such as concentration of Avastin in a nasal spray.
If Avastin is added to a saline solution and compounded as a nasal spray what would the shelf life be of this product?
How much and how often should the nasal spray be administered?
I am looking at this product to treat hht nosebleeds only.
I have hht in my nose only and am interested in the Avaston treatment.
Please tell me if this works, side effects and if this is something that will be supported through a trial or /and what the cost is?
The laser surgeries do not last long, only a bandage for a few months
Thank you
I have been taking Advastin for several years now because of chronic nose bleeding.
And it has been working wonders for me. Along with having Vonwillibrands. Two hereditary bleeding disorders.
My concern is when I retire Medicare may not pick this up.
Just last week I had intranasal laser with avastin injections. 2nd operation 9 years apart. Had 80 iron infusions in that time but managed an active lifestyle
Looking forward to a lengthy break from nose bleeds
Now 60
Lived with my special condition for as long as I remember
Stay positive and manage the anemia
Does anyone know if the rate of deterioration is linea or exponential with age ?
I have had nose bleeds all of my life but it was never on a daily basis. As I got older I discovered that I had HHT. My nose bleeds sped up so that sometimes I could have one to three nose bleeds a day. Cauterization did nothing for me. I had tried using vaseline and oil inserted into the nose using Q-tips. Although it helped it never really gave me total relief from multiple nose bleeds. One day I came across a nasal rinse that I apparently got as a sample at a health fair so I decided to try it for my nose bleeds. It is called “nasopure” (I ordered it on-line because I could not find that specific brand in the local drug stores etc. I rinse my nasal cavity every morning and then blow my nose to get all of mucus etc out, and follow that by dipping a Q-tip into a bottle of thick castor oil and rub that inside my nose. I also put vaseline into the nose in addition to the castor oil. That has been my salvation for keeping my nose bleeds at bay. Although I still get a nose bleed from time to time it is not on a daily basis or multiple times a day like it use to be. Just wanted to let this be known what has helped me.
My name is Martin and I was diagnosed with hht in
1996 when I was 25. I’m now 51 and am getting Avastin for the first time. I pray that it will help me
have more endurance and less pressure on my heart because of the increased red blood cells which make my blood very thick. Nosebleeds were a huge problem for me until I started taking curcumin. It’s a vitamin supplement that I buy through Amazon. I rarely get nosebleeds now. I just wanted to put it out there. Brand is aSquared nutrition- Tumeric Curcumin with Bioperine. I take two capsules a day as the label recommends. When I first started my nosebleeds got worse but then lessened after about two months. That was about four years ago. So much better now.
So, Say a patient with a dvt has HHT. They can REALLY BLEED ON THINNERS. Take it from me I’ve experienced it. How would a person treat the DVT