The Call of the Lung & Blessings Counted

2016 is the year my largest PAVM, first detected and treated in 1993, decided to fully challenge my life. Over the previous four years, my HHT interventional radiologist had made a valiant effort to close this PAVM, but this singular cluster of mixed up pathways now threatened my existence.
At 5 p.m. on a Friday evening in early February, I started to cough up more blood than was normal for me, even having experienced multiple PAVMs which required embolization. I didn’t say much to my daughter, but I felt like this could be of serious consequence.
Normally, if I had some hemoptysis, it would stop in an hour or two and would be fairly light. The next morning, when I woke up after a brief hour or two of sleep, I was still coughing up large amounts of blood. I paced the floor for an hour and finally woke my daughter. In an attempt not to frighten her, I calmly said that when she was up and ready, we would drive to the hospital.
It wasn’t long after arriving in the emergency room I was admitted to the hospital. The stay there lasted 10 days. I needed surgery to remove the bottom lobe of my right lung. There were no more non-surgical interventions to resolve this bleed.
Actually, the surgeon suggested I not deliberate too long as he had witnessed others in similar circumstances who did not benefit from waiting. I was convinced. They had looked at this weak point from every direction possible. I agreed to go forward with the surgery. In fact, it had been suggested by my HHT doctor after an embolization that I might be a candidate for this larger procedure in the future. I had no idea my “HHT future” would accelerate its way into my life that quickly.
The operation was a great success. They removed the lower lobe of my right lung, where this PAVM had been in residence. When the surgeon’s partner showed me the pictures of the offending spot on the removed lobe, I couldn’t even count all the coils left behind from previous interventions. The area around the PAVM had dead lung tissue and was toxic. Frightening!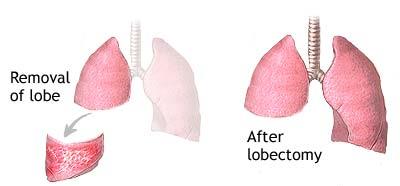
My hospital recovery went superbly, but my heart kept going into AFIB, atrial fibrillation. After two and a half months, I resumed my normal AFIB medicine and seem to be fine now. Another post surgery effect hit my gastrointestinal tract. I have had many GI upsets. After many months of trying to figure it out, I enlisted a GI doctor. I am still working with her, but I have generally concluded that I can no longer tolerate what I used to eat. Therefore, I am trying a gluten, GMO, dairy and soy-free diet.
Things have quieted down for me. I may never know the exact culprit, but I am still tweaking things. After all, there is no test for merely having gluten intolerance, yet reportedly 15 percent of the population has this. And GMOs, who knows? My HHT and its treatments have both directly and indirectly affected many other facets of my health.
It has been six months since my surgeon told me I’d get 90 percent of my lung power back. I have been able to increase my walks threefold and can actually sing again in church without feeling short of breath. I am so glad I was able to get immediate attention when this life-threatening event occurred. Had I waited, the outcome could had been dire.
Blessings counted!
